The article underscores the importance of the Standard Liver Blood Test UK as a critical tool for diagnosing iron deficiency, which is a common health issue in the UK. Unlike other tests that measure haemoglobin or serum iron, the Standard Liver Blood Test includes ferritin level testing, which provides a more accurate assessment of both acute and chronic iron status. Ferritin serves as a key biomarker for iron reserves, and its measurement in the SLBT UK allows for simultaneous evaluation of iron status and liver function. This test is crucial for differentiating iron deficiency anaemia from other conditions that may have similar symptoms, such as those related to chronic diseases or inflammation. Early diagnosis through this test enables prompt intervention and helps prevent the complications associated with iron deficiency. It is recommended that individuals concerned about their iron health consult healthcare providers for insights into their iron status via the Standard Liver Blood Test UK, which can be conducted without the need for invasive procedures. Understanding the role of ferritin within the context of this test is essential for effective management of iron-related health issues, with personalized management plans developed in consultation with healthcare professionals being key to treatment. Regular monitoring, dietary changes, and possibly iron supplements or intravenous iron therapy can help manage iron deficiency, making the Standard Liver Blood Test UK an indispensable diagnostic tool for maintaining overall health.
Navigating iron deficiency can be a complex task, yet understanding one’s iron status is crucial for maintaining overall health. In the UK, the Standard Liver Blood Test plays an pivotal role in this process, particularly through ferritin level testing. This article delves into the significance of ferritin as a biomarker within the context of the UK’s standard health screenings, offering a clear guide to interpreting results and managing iron deficiency detected via this essential test.
- Deciphering Iron Health: The Role of Ferritin Level Testing in the UK
- Understanding Ferritin as a Biomarker for Iron Status within the Standard Liver Blood Test UK
- Practical Guide to Interpreting Ferritin Results and Managing Iron Deficiency Identified through the Standard Liver Blood Test UK
Deciphering Iron Health: The Role of Ferritin Level Testing in the UK

Iron deficiency is a prevalent concern in the UK, with proper diagnosis being a critical step towards effective treatment and management. Ferritin level testing plays a pivotal role in this process, serving as an indicator of iron stores in the body. Unlike haemoglobin or serum iron tests which provide a snapshot of current iron levels, ferritin acts as a more reliable biomarker due to its ability to reflect both acute and chronic iron status. It’s an acute-phase protein, meaning it can rise in the event of inflammation or infection, but it remains a valuable tool in the context of diagnosing iron deficiency across various demographics.
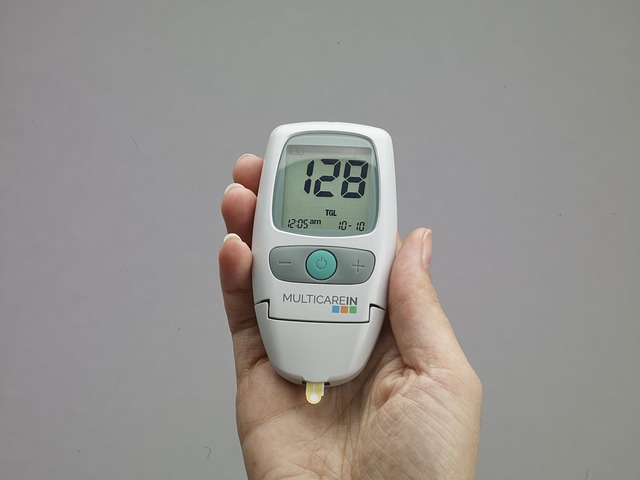
In the UK, the Standard Liver Blood Test is often the first step healthcare providers take when assessing liver health and, incidentally, indirectly evaluating iron status as ferritin is included in this panel. This test measures the amount of ferritin in the blood, which can help differentiate between iron deficiency anaemia and other conditions that may cause anaemia, such as chronic disease or inflammation. The results from this test are crucial for early diagnosis and management, enabling timely intervention to prevent complications associated with iron deficiency. For those concerned about their iron health, discussing the Standard Liver Blood Test with a healthcare provider can be an important first step towards understanding one’s iron status and taking appropriate action.
Understanding Ferritin as a Biomarker for Iron Status within the Standard Liver Blood Test UK
Iron is a critical element for haemoglobin production and oxygen transport in the body, making iron status a vital component of overall health. Ferritin, a protein that stores iron, serves as an excellent biomarker for assessing iron reserves within the body. It is particularly notable within the context of the Standard Liver Blood Test (SLBT) UK, which routinely includes ferritin levels to evaluate both iron status and liver function. This dual function of ferritin in the SLBT UK is significant as it provides healthcare professionals with a comprehensive overview of an individual’s iron stores and hepatic health simultaneously.
The inclusion of ferritin in the SLBT UK is a testament to its reliability as a biomarker. Elevated ferritin levels can indicate either high iron stores or inflammation, which may be associated with liver conditions. Conversely, low ferritin levels can suggest iron deficiency or depleted iron reserves. The sensitivity of ferritin to both iron metabolism and inflammatory responses makes it an invaluable tool for diagnosing iron-deficiency anaemia, a common condition that can affect individuals of all ages. By identifying this deficiency early through the SLBT UK, healthcare providers can initiate appropriate treatment plans, thereby preventing the progression of anaemia and its potential complications. Understanding ferritin’s role in the SLBT UK is crucial for patients and clinicians alike, as it facilitates early detection and management of iron-related health issues.
Practical Guide to Interpreting Ferritin Results and Managing Iron Deficiency Identified through the Standard Liver Blood Test UK
Understanding your ferritin levels is crucial for managing iron deficiency, a condition that can lead to anemia and various health issues. The Standard Liver Blood Test UK is routinely used as a screening tool to assess liver function but also provides valuable insights into iron status. Ferritin, a protein that stores iron in the body, is measured during this test. Normal ferritin levels can vary depending on age and sex; typically, levels for men are higher than those for women. Interpreting ferritin results requires an understanding of these normal ranges. A ferritin level below 30 micrograms per liter (mcg/L) often indicates iron deficiency, while levels between 30 to 150 mcg/L suggest adequate iron stores for most menstruating women and 12-300 mcg/L for men. If your ferritin results fall within these ranges but you exhibit symptoms of iron deficiency, such as fatigue or paleness, further evaluation and management may be necessary.
Managing iron deficiency identified through the Standard Liver Blood Test UK involves several steps. If your ferritin levels are low, dietary changes can be beneficial. Incorporating more iron-rich foods like lean red meat, dark green leafy vegetables, iron-fortified cereals, and legumes can help increase your iron intake. Additionally, taking an iron supplement, as prescribed by a healthcare provider, is often essential to restore iron levels. It’s important to monitor ferritin levels regularly after initiating treatment to ensure that iron stores are returning to normal. In cases where dietary changes and supplementation are insufficient, medical interventions such as intravenous iron therapy may be required. Consulting with a healthcare professional is key to developing an effective management plan tailored to your individual needs.
In conclusion, ferritin level testing as part of the Standard Liver Blood Test in the UK is a pivotal tool for diagnosing iron deficiency. This article has elucidated its significance, offering insights into how healthcare professionals can effectively interpret ferritin results and manage iron deficiency. By integrating this biomarker into routine health assessments, individuals can proactively address their iron status, thereby improving overall well-being and reducing the risk of associated complications. It is imperative for those experiencing symptoms suggestive of iron deficiency to consult healthcare providers for the Standard Liver Blood Test, which includes ferritin measurement, to ensure accurate diagnosis and appropriate treatment. Recognizing the importance of early detection and intervention can significantly enhance health outcomes within the UK population.